keratoplasty
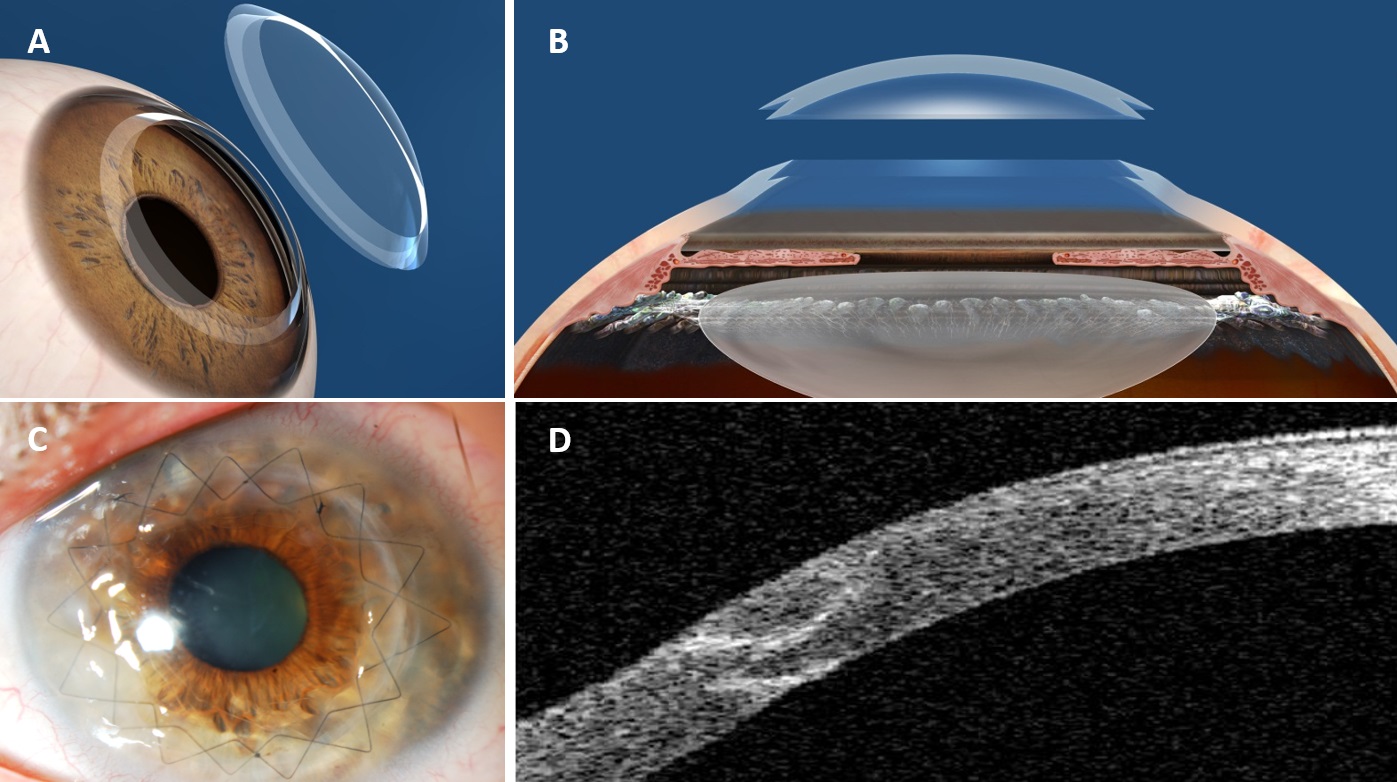
Various pathologies such as keratoconus can lead to permanent vision loss. In such critical cases, it is necessary to perform a corneal transplantation. This type of surgery is commonly called keratoplasty.
The procedure involves replacing a damaged cornea with a healthy one from a donor. Also known as penetrating keratoplasty, corneal transplantation has given many patients the chance to regain good vision after suffering from corneal opacity.
Studies have shown a success rate of over 66% for this operation on a five-year follow-up of patients suffering a damaged cornea. Hence, keratoplasty is considered a safe treatment to cure several severe vision-related pathologies.
- Penetrating keratoplasty is an outpatient procedure, meaning that patients can go home the same day as their surgery. Before the penetrating keratoplasty procedure begins, a local or general anesthesia is administered. Your eye surgeon will then use a trephine, a circular cutting device, to cut the donor cornea to the exact shape and size that is needed.A second trephine is then used to remove a matching portion of the patient’s cornea, at which point the donor tissue is positioned and sewn into place. The physician will then apply antibiotic eye drops and cover the eye with a protective shield.
A penetrating keratoplasty is an outpatient procedure, meaning that patients are able to go home the same day as their surgery. Most patients will return the following day for a post-operative appointment.
Following a corneal transplant, patients are given medicated eye drops to take in the subsequent weeks and months to aid the healing process. After the procedure, patients may find that their vision is blurry while the eye adjusts to the new cornea. While recovery times vary, most patients find that their eyes heal and vision improves over the course of a few months after surgery.
During the days following the procedure, it is important to protect the eye as much as possible. Your doctor may recommend that you wear a protective shield during this time. As the eye continues to heal in the following weeks and months, we recommend avoiding activities which may cause trauma to the eye, such as playing sports.
The corneal transplant may be technically performed perfectly, and the transplant may be working as well as it can be, but other eye problems may limit the quality of a person’s vision post-operatively. The new cornea may have a significant amount of astigmatism and glasses or special contacts may be required to improve vision. Other eye diseases such as macular degeneration, diabetic retinopathy, or glaucoma may also limit the patient’s quality of vision and prevent the patient from seeing 20/20.
Risks
Risks of PK are similar to those of other intraocular procedures including infection, inflammation, glaucoma, bleeding, retinal detachment, but additionally include graft rejection and detachment or displacement of the graft. Corneal rejection occurs in about 20 percent of cases. Graft failure can occur at any time after the cornea has been transplanted, even years or decades later.
Signs and Symptoms of Cornea Rejection
The body’s immune system may mistakenly attack the donor cornea in some cases. This is called rejection, and it requires further medical treatment or another corneal transplant. Signs and symptoms of cornea rejection include loss of vision, pain, redness, or sensitivity to light. Rejection occurs in 20 percent of cornea transplants. If the first transplant is rejected, certain patients may need a second transplant. A repeat transplant carries a higher rate of rejection than the first.
