Intracytoplasmic Sperm Injection (ICSI)
For people experiencing infertility, intracytoplasmic sperm injection (ICSI) may lead to a successful pregnancy. This type of in vitro fertilization (IVF) is most helpful when there are male infertility issues. Your healthcare provider injects sperm into an egg to aid conception. Pregnancy may happen after an embryo transfer.
Intracytoplasmic sperm injection (ICSI) is an infertility treatment. It involves injecting live sperm into a person’s eggs in a laboratory. This procedure can create an embryo (fertilized egg). ICSI is a form of in vitro fertilization (IVF). Healthcare providers most commonly use ICSI when male infertility. affects a person’s ability to conceive a child.
Intracytoplasmic (IN-truh-sahy-tuh-PLAZ-mik) refers to the fact that the sperm injection takes place inside an egg’s cytoplasm. This is the gel-like substance in the center of an egg, made up of water, salt and other molecules.
ICSI is a type of IVF. With traditional IVF, your healthcare provider places thousands of sperm next to an egg on a laboratory dish. Whether one of the sperm penetrates the egg to fertilize it is left up to chance. If none of the sperm fertilize the egg, conception (also called fertilization) doesn’t occur.
ICSI promotes fertilization through the direct injection of a single sperm into a single egg. Still, ICSI doesn’t guarantee fertilization.
In both ICSI and traditional IVF, your healthcare provider implants the fertilized egg (embryo) into your uterus. Pregnancy occurs if the embryo attaches to the lining of your uterus.
Both ICSI and IVF use assisted reproductive technology (ART) to treat infertility (difficulty getting pregnant). ART refers to lab-based fertility treatments that use eggs and sperm outside of the human body to start conception (pregnancy).
Approximately 6 in 10 IVF procedures take place using ICSI. Your chances of having a successful pregnancy are the same with ICSI as with traditional IVF. It’s estimated that 50% to 80% of ICSI attempts result in fertilization.
ICSI is most helpful for people experiencing male infertility. Your healthcare provider may recommend ICSI if a person has:
- Anejaculation (inability to ejaculate).
- Blockage in their male reproductive system.
- Low sperm count.
- Poor sperm quality.
- Retrograde ejaculation (semen flows backward into their bladder).
You may also need ICSI if:
- Traditional IVF hasn’t led to the creation of embryos.
- The person supplying the eggs is older than 35.
- You’re using previously frozen eggs or sperm (cryopreservation) to try to conceive.
You may see an Ob/Gyn who’s also a reproductive endocrinologist. These medical doctors treat disorders of the endocrine system that affect reproduction. They specialize in diagnosing and treating infertility, as well as fertility preservation.
Before ICSI takes place, your healthcare provider must collect the eggs and sperm.
These steps take place for egg retrieval:
- Ovulation induction (also called ovarian stimulation): The person supplying the eggs receives medication injections for eight to 14 days. This stimulates your ovaries to produce multiple eggs at once to mature. Next, a Lupron or human chorionic gonadotropin (hCG) injection will assist with final maturation of the eggs.
- Egg retrieval: Your healthcare provider uses transvaginal ultrasound technology to guide the insertion of a thin needle through the wall of your vagina into your ovaries. This step is done with a mild anesthetic, so there isn’t any pain. A suction device connected to the needle draws out and collects the eggs.
Unless you’re using frozen sperm, sperm collection takes place on the same day as the egg retrieval. The person supplying the sperm:
- Abstains from sex and masturbation (no ejaculation) for two to three days prior to the sperm collection.
- Masturbates at home or in a private room at a fertility clinic, collecting the ejaculate into a lab-provided container. The specimen must be received by the laboratory within 60 minutes from ejaculation.
A semen analysis takes place immediately to check sperm volume, mobility and quality. People who experience azoospermia, anejaculation or retrograde ejaculation may need a procedure to collect sperm. This is also true for people who undergo an unsuccessful vasectomy reversal. Procedures like electroejaculation and microscopic testicular sperm extraction may take place in a hospital instead of a fertility clinic. A lab may freeze and store the sperm
(sperm banking) for later IVF use at the clinic.
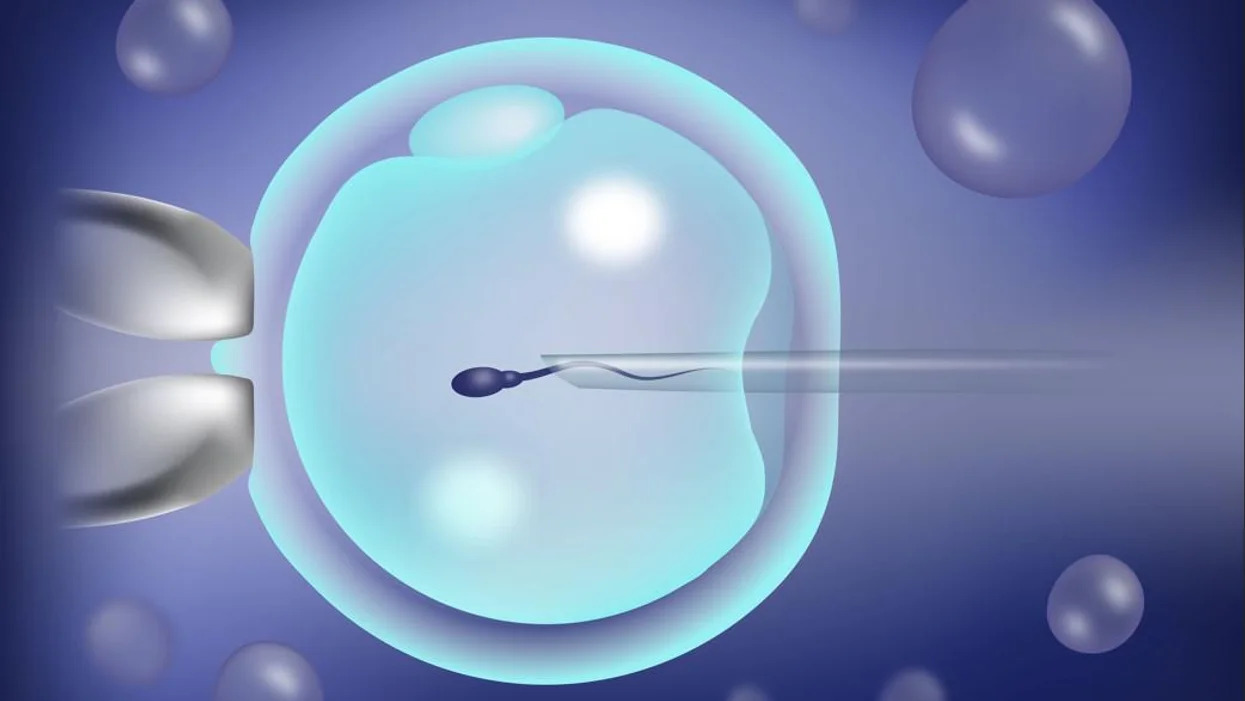
During ICSI, your healthcare provider:
- Uses a pipette (small glass tube with a suction bulb) to hold the mature egg in place on a lab dish.
- Immobilizes and picks up one sperm using a thin needle.
- Inserts the needle into the egg to reach the cytoplasm.
- Injects the sperm into the cytoplasm.
- Withdraws the needle from the egg.
After ICSI, your healthcare provider monitors the fertilized egg in the laboratory for signs of successful fertilization. Within five to six days, a healthy fertilized egg should divide into cells, forming a blastocyst. Your healthcare provider will evaluate the blastocyst’s size and cell mass to determine when it’s most likely to lead to a pregnancy.
An embryo transfer occurs on either on the fifth or sixth day following the egg retrieval procedure or commonly the transfer is delayed for a month or even years. Your doctor will discuss the timing of your embryo transfer with you. Using ultrasound technology, your healthcare provider will insert a catheter (long, thin tube) into your vagina and inject the embryo into your uterus. For pregnancy to happen, the embryo needs to implant (attach) to your uterus. Your healthcare provider may recommend waiting at least two weeks before taking a pregnancy test.
Compared to traditional IVF, ICIS appears to be more successful in helping those experiencing male infertility become parents. Some centers do ICSI for all people, regardless of infertility diagnosis.
These complications may occur with ICSI:
- Damage to some or all of the eggs during needle penetration.
- An egg doesn’t fertilize after the sperm injection.
- An embryo stops developing in the lab or after embryo transfer.
In the U.S., approximately 2% of babies have congenital conditions (meaning born with a health condition). An additional 1% of children conceived with ICSI have congenital conditions. Medical experts think the underlying cause of infertility may contribute to these problems — not the fertility treatment itself. And this risk is relatively small given that birth defects occur in 2% of newborns every year.
ICSI may slightly increase a child’s risk of:
- Angelman syndrome.
- Autism.
- Beckwith-Wiedemann syndrome(a growth disorder).
- Disorders of sex differentiation.
- Hypospadias.
- Intellectual disabilities.
