Diabetes-Related Macular Edema
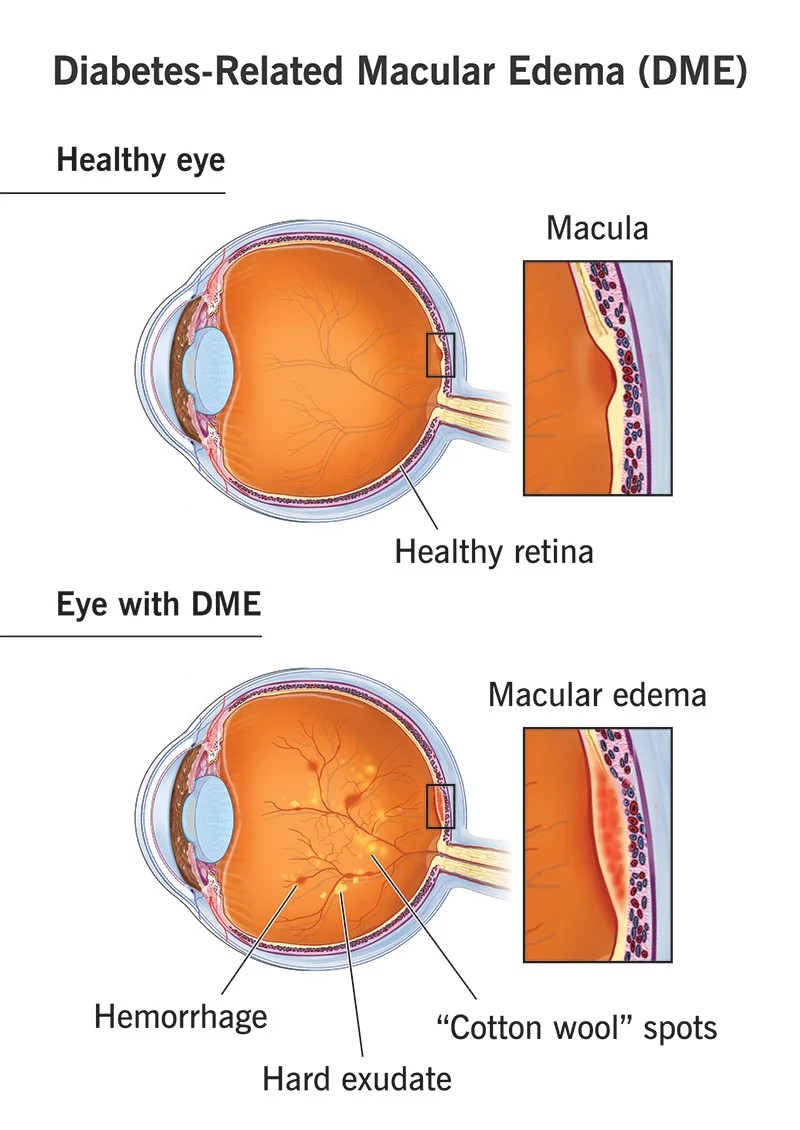
Diabetic macular edema (DME) is an eye condition that affects some people with diabetes. It’s characterized by fluid buildup in the macula — the area of the retina that’s responsible for detailed vision right in front of you.
When fluid leaks into the macula from nearby blood vessels, it swells, causing blurry vision and other visual changes, such as colors looking dull or faded.
The severity of diabetic macular edema symptoms can range from mildly blurry vision to severe loss of central vision that makes daily activities difficult.
Diabetic macular edema can affect people with either type 1 or type 2 diabetes. It’s strongly related to high blood sugar levels and a longer history of diabetes, as well as high blood pressure and high cholesterol
When diabetic macular edema is caught early and treated, vision loss can usually be stopped and sometimes even reversed.
Diabetes-related macular edema (DME) is swelling in the macula, or central, part of the retina of your eye. Your retina is in the back of the eye and is the part of your eye that houses the light-sensing cells. Your macula lets you see fine details.
You can get DME if you have diabetes-related retina disease . Diabetes affects the blood vessels in your eyes, making them weaker and more likely to leak blood. It may also cause new and more fragile blood vessels to grow where they shouldn’t grow.
About 1 in 14 people with diabetes develop diabetes-related macular edema. In the U.S., more than 37 million adults have diabetes currently.
The signs and symptoms of diabetes-related macular edema may include:
- Blurry vision or double vision
- Difficulty seeing colors.
- Dark spots (scotomas).
- Straight lines that you see as bent or curved.
- Difficulty seeing when there’s a glare or bright light.
- Seeing an object as being a different size when you look at it with only one eye and then the other.
- Diabetes-related macular edema happens when high blood sugar levels affect the blood vessels in your eyes. Your blood vessels leak, which causes fluid to build up and thicken your retina.Issues with blood vessels happen to people who have diabetes-related retinal disease or diabetes-related retinopathy (DRR). Blood vessels become weak and form pouches. The pouches leak. This is non-proliferative DRR.If you begin to grow new blood vessels in your eyes that don’t belong there, you have proliferative DRR. These new blood vessels aren’t as strong as they should be, so they also leak and allow blood to build up in your macula and retina.A serious complication of untreated diabetes-related macular edema is vision loss.
You can’t see swelling in your retina, but your eye care specialist can see this when they do a thorough eye Examination. This is one reason that you need to have regular eye exams. Following an eye exam schedule is especially important if you have diabetes.
What tests will be done to diagnose diabetes-related macular edema?
In addition to the eye exam, which includes a slit lamp exam, your provider may use the following tests to diagnose and monitor DME:
- Optical coherence tomography : This imaging test can measure the thickness of your retina and optic nerve.
- Fluorescein angiography: This imaging test shows the blood vessels in your retina.
- Amsler grid: This test uses a grid of horizontal and vertical lines in a visiual field test.
Treatment options for DME have improved. In fact, some newer medications work well enough to reverse the damage in some cases.
One form of treatment blocks vascular endothelial growth factor (VEGF), a protein that helps new blood vessels grow. Steroids that manage inflammation are another form of treatment that’s applied to your eyes.
In addition, your provider will work with you to manage your blood sugar levels and your blood pressure. This process might involve other types of medications.
Drugs that treat diabetes-related macular edema
One of the ways that providers treat DME is with a series of intravitreal injections of medications. These medications include:
- Aflibercept (Eylea®).
- Bevacizumab (Avastin®).
- Faricimab-svoa (VABYSMO®).
- Ranibizumab (Lucentis®).
- Dexamethasone (Ozurdex®).
- Fluocinolone acetonide (Iluvien®).
Ozurdex and Iluvien are steroid implants that your provider injects into your eye.
Procedures that treat diabetes-related macular edema
Providers may use laser therapy (photocoagulation) to seal the blood vessels in your eyes to stop the leakage.
Another procedure that your provider might suggest is a vitrectomy. This surgery can remove scar tissue and cloudy vitreous fluid from your eye.
Complications or side effects of treating diabetes-related macular edema
The chance of complications with DME treatments is low, but there are always risks, such as infection, when anything penetrates your eye.
Other potential complications could be that you develop air bubbles in your eyes after the injections. These air bubbles will be similar to floaters and resolve within a few days.
Likely side effects of injections include eye redness and irritation, which can be from the cleaning solution used prior to the injection to reduce infection risk. Using artificial tears on the day of injection can help with irritation.
Steroid treatments may have additional complications, such as cataracts or higher eye pressure .
Normally, you don’t have pain with diabetes-related macular edema, so you won’t really “feel better” after having injections. The treatments should stop or reverse damage to your macula, retina and vision. You don’t have to wait to go back to work or school.
Recovering from a vitrectomy will take longer than other therapies. You’ll need to take off for two to four weeks.
You may be able to reduce your risk of developing diabetes-related macular edema by:
- Managing diabetes.
- Managing other chronic conditions, such as high blood pressure (hypertension)
- Getting regular eye exams.
- Quitting smoking.
- Eating a healthy diet.
- Getting regular physical activity.
If you have DME and you have successful treatments, your outlook is good. Some of the newer medications seem to restore some lost vision, but this is primarily when your provider can diagnose and treat DME early.
Without treatment, DME can result in a significant loss of vision, which could have an impact on the way that you live your life.
Although DME is a condition that affects your eyes, you can help yourself by taking care of your entire body.
- Do your best to manage chronic conditions like diabetes, high blood pressure, obesity or overweight and high cholesterol.
- Eat a healthy diet and get enough exercise.
- Don’t smoke.
- See your eye care provider regularly, following whatever schedule they advise.
- If you have sudden vision loss or severe eye pain, contact your provider or go to an emergency room.
- What should I know about diabetes-related macular edema?
- What treatment do you suggest?
- What are the side effects or complications of this treatment for DME?
- How often should I get eye exams?
- What do you consider an emergency with DME?
